Models Forced Expiratory Volume procedure using the linear one chamber compartment model taken from Bates (ch. 3)
Description
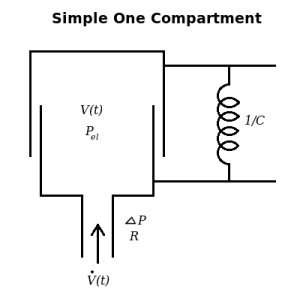
This model adapts the single compartment lung as developed by Bates to the forced expiratory volume (FEV) procedure. The model includes a resistance term (represented by airway resistance) and a spring recoil term (spring resistance represented by 1 / lung compliance, 1/C) for the lung. Several commonly used lung volumes have been calculated and reported. This model can be modified to add to a larger model or can be used alone as a simple model. A data set has been added and a fit has been attempted. This model has several problems. First, it cannot be fit to a real data curve, thus invalidating the model for real world use. A more accurate model has been created using the Maxwell viscoelastic system as also developed by Bates (insert model number, Bates pg 117-118). The viscoelastic behavior contributed by the addition of the Maxwell body gives the more accurate model a 2-component outflow and the ability to fit to actual data. However, the following problems are shared by both models. The second problem is that the driving pressure of the system is external, not from the chest wall, and therefore acts like a respirator pumping up the lung with positive pressure and sucking the air out with negative pressure, the reverse of normal ventilation. This is the opposite of the "forced expiration" compressing the chest and raising intrapleural pressure. The third problem is that the compliance, C1, is constant instead of being functions of the volume. In reality the FEV ends, at Vlung = Functional Reserve Capacity - Expiratory Reserve Volume = Residual Volume, when the force of chest muscle contraction cannot make the chest smaller (equivalent to compressing the spring further). The passive pressure-volumes curves should be concave upward for both chest and lungs at volumes above FRC, At FRC the chest recoil is toward enlargment and the lung recoil is toward shrinkage, so the combination produces a negative intrapleural pressure at rest. Fourth, air is assumed to be incompressible. In reality air flow inward through the mouth is less than flow into the lungs because of the additional volume contributed by water vapor pressure rising to 47 mmHg. With an FEV the volume is compressed, often by 1/8th, i.e. 100 mmHg exhalation pressure added to 760 mmHg.
Figure
Equations
The equations for this model may be viewed by running the JSim model applet and clicking on the Source tab at the bottom left of JSim's Run Time graphical user interface. The equations are written in JSim's Mathematical Modeling Language (MML). See the Introduction to MML and the MML Reference Manual. Additional documentation for MML can be found by using the search option at the Physiome home page.
- Download JSim model MML code (text):
- Download translated SBML version of model (if available):
We welcome comments and feedback for this model. Please use the button below to send comments:
J.H.T. Bates. Lung Mechanics: An Inverse Modeling Approach. Cambridge University Press, (2009) Chapter 3: 37-44, Chapter 7: 117-118.
Please cite https://www.imagwiki.nibib.nih.gov/physiome in any publication for which this software is used and send one reprint to the address given below:
The National Simulation Resource, Director J. B. Bassingthwaighte, Department of Bioengineering, University of Washington, Seattle WA 98195-5061.
Model development and archiving support at https://www.imagwiki.nibib.nih.gov/physiome provided by the following grants: NIH U01HL122199 Analyzing the Cardiac Power Grid, 09/15/2015 - 05/31/2020, NIH/NIBIB BE08407 Software Integration, JSim and SBW 6/1/09-5/31/13; NIH/NHLBI T15 HL88516-01 Modeling for Heart, Lung and Blood: From Cell to Organ, 4/1/07-3/31/11; NSF BES-0506477 Adaptive Multi-Scale Model Simulation, 8/15/05-7/31/08; NIH/NHLBI R01 HL073598 Core 3: 3D Imaging and Computer Modeling of the Respiratory Tract, 9/1/04-8/31/09; as well as prior support from NIH/NCRR P41 RR01243 Simulation Resource in Circulatory Mass Transport and Exchange, 12/1/1980-11/30/01 and NIH/NIBIB R01 EB001973 JSim: A Simulation Analysis Platform, 3/1/02-2/28/07.