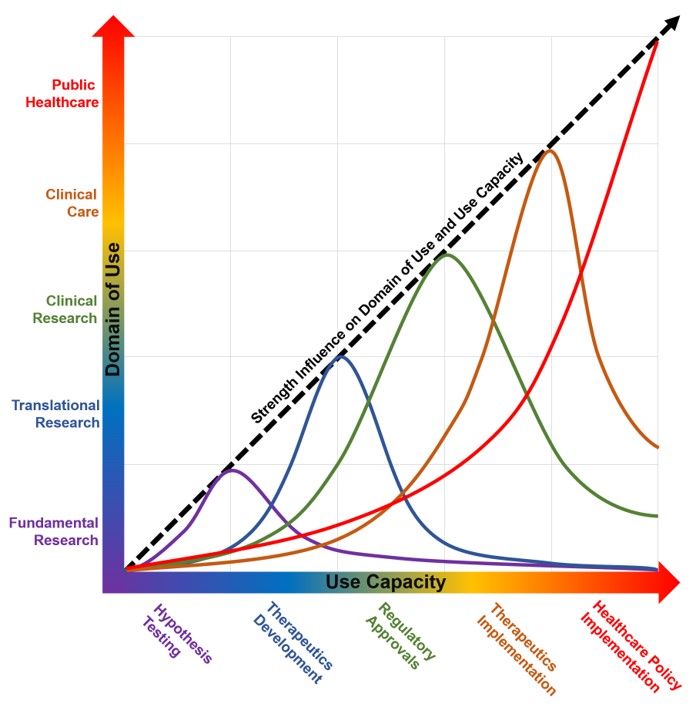
The complexities of modern biomedicine are rapidly increasing. Thus, modeling and simulation have become increasingly important as a strategy to understand and predict the trajectory of pathophysiology, disease genesis, and disease spread in support of clinical and policy decisions. In such cases, inappropriate or ill-placed trust in the model and simulation outcomes may result in negative outcomes, and hence illustrate the need to formalize the execution and communication of modeling and simulation practices. Although verification and validation have been generally accepted as significant components of a model’s credibility, they cannot be assumed to equate to a holistic credible practice, which includes activities that can impact comprehension and in-depth examination inherent in the development and reuse of the models. For the past several years, the Committee on Credible Practice of Modeling and Simulation in Healthcare, an interdisciplinary group seeded from a U.S. interagency initiative, has worked to codify best practices. Here, we provide Ten Rules for credible practice of modeling and simulation in healthcare developed from a comparative analysis by the Committee’s multidisciplinary membership, followed by a large stakeholder community survey. These rules establish a unified conceptual framework for modeling and simulation design, implementation, evaluation, dissemination and usage across the modeling and simulation life-cycle. While biomedical science and clinical care domains have somewhat different requirements and expectations for credible practice, our study converged on rules that would be useful across a broad swath of model types. In brief, the rules are: (1) Define context clearly. (2) Use contextually appropriate data. (3) Evaluate within context. (4) List limitations explicitly. (5) Use version control. (6) Document appropriately. (7) Disseminate broadly. (8) Get independent reviews. (9) Test competing implementations. (10) Conform to standards. Although some of these are common sense guidelines, we have found that many are often missed or misconstrued, even by seasoned practitioners. Computational models are already widely used in basic science to generate new biomedical knowledge. As they penetrate clinical care and healthcare policy, contributing to personalized and precision medicine, clinical safety will require established guidelines for the credible practice of modeling and simulation in healthcare.